Mental Health And the War on Drugs
“What did not occur with the closing of the huge mental health facilities was the creation of a new set of institutions that would respond to the needs of people who have mental or emotional challenges, and we’re living with the consequences of that now. When we talk about the possibility of closing down prisons, we cannot simply close down prisons, but we have to create the kind of institutions that will allow people to change and to heal and to develop.”
co-occurring mental illness and substance use disorders
The co-occurrence of substance use disorders among individuals with mental illness is common. This co-occurrence is particularly concerning because individuals struggling [or "diagnosed"] with both mental illness and substance use disorders experience more adverse outcomes than those with mental illness or substance use disorder alone, including more frequent relapse and hospitalization, premature death, and a higher rate of infectious diseases, unemployment, homelessness, and incarceration.
What Is Comorbidity?
The term “comorbidity” describes the presence of two or more disorders or illnesses in the same person. They can occur at the same time or one after the other. Comorbidity also implies interactions between the illnesses that can worsen the course of both.
the impact of mental health disorders in New York City
Major depressive disorder is the single greatest source of disability in NYC. At any given time over half a million adult New Yorkers are estimated to have depression, yet less than 40% report receiving care for it. Mental
illness and substance use disorders are among the leading contributors to the disease burden for New Yorkers, with depressive illness the single largest contributor after heart disease. If the impact of alcohol use
disorders and other substance use disorders were added together the combined group would be the second leading contributor to overall disease burden in New York City.
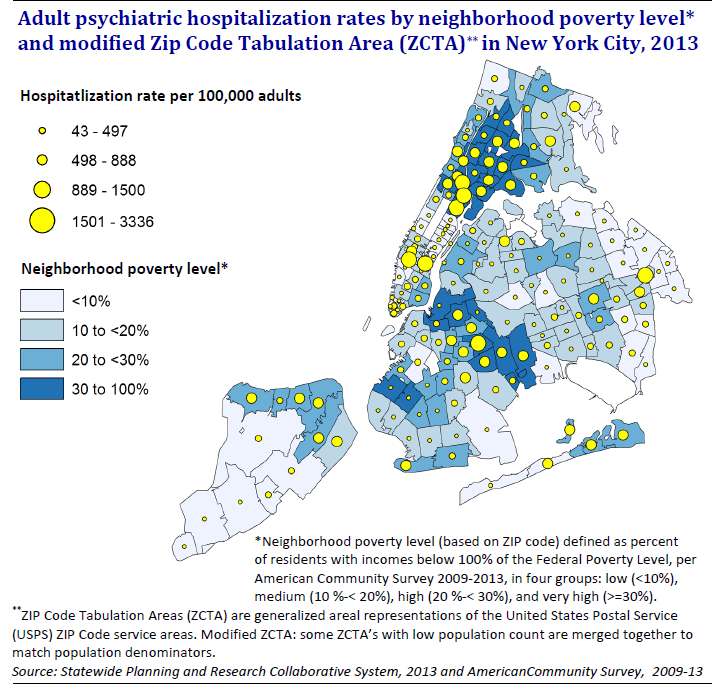
Race, poverty and mental health
Despite the fact that people of color and those in poverty bear the greatest mental health burden, they are among the least likely to get help.
African Americans, Latinos and Asians are less likely than whites to receive mental health treatment in the form of counseling or medication, according to a survey of NYC residents.
National studies suggest that African Americans can be half as likely as whites to receive community-based mental health care, but as much as twice as likely to be hospitalized. The likelihood of someone having a psychiatric hospitalization in New York City varies dramatically by neighborhood and income. People from the city’s lowest income neighborhoods are twice as likely to be hospitalized for mental illness compared to residents from the highest income neighborhoods.